
Nail psoriasis is a special form of psoriasis in which the fingernails and / or toenails are affected. Doctors call this type of disease psoriatic onychodystrophy (from the Greek.onychos- nail,dis- violation,trophe- food).
From this article, you will learn about the causes of the development of nail psoriasis, its symptoms, which do not always unambiguously indicate the correct diagnosis, as well as dangerous misconceptions about this form of the disease.
Note.There are many photographs in the article that can scare an unprepared reader.
Where do nails grow from?
To understand the problem of nail psoriasis, it is important to understand how the so-called nail system works.
The nail has two functions: working and aesthetic. First, the nail protects the fingertips from damage, increases accuracy and sensitivity when working with small objects, can be a weapon of attack or defense, and finally, with the help of the nails it itches. Secondly, the aesthetic or cosmetic function of the nails is also important, especially for women.
Nails are formed from the outer layer of the skin: the epidermis. The nail apparatus includes:
- nail plate - directly the nail itself,
- matrix - produces the nail plate,
- the nail hole, or lunula, is the only visible part of the matrix, this is a white moon-shaped area at the base of the nail plate,
- eponychium - a nail roller that protects the matrix from above from damage,
- nail bed - located under the nail plate and is responsible for its attachment to the nail phalanx of the finger,
- hyponychia: the transition zone between the nail bed and the skin of the fingertip.
Causes and mechanism of development of nail psoriasis
In its course - with periodic exacerbations and remissions - psoriasis on the nails resembles a vulgar form of the disease.
Nail psoriasis is believed to develop for the same reasons and in the same pattern as typical psoriatic rashes. Among these reasons, external and internal factors are distinguished.
The main intrinsic factor is genetic predisposition. External causes are numerous and include, for example, injuries, poor diet, intoxicants (alcohol and tobacco), infections, and some medications.
The standard mechanism of development of nail psoriasis under the influence of these reasons can be briefly described as follows:
- Provoking factors, such as trauma, activate immune cells.
- Activated immune cells migrate to the area of the nail matrix or nail bed.
- Immune inflammation develops in these areas.
- The division of skin cells is abruptly accelerated and their maturation is stopped.
- There are characteristic symptoms of psoriasis on the nails.
Also, the cause of nail psoriasis can be considered as a consequence of the body's inability to adapt to adverse environmental conditions. According to this view, the main cause of psoriasis is an evolutionarily alien habitat.
Consequently, this evolutionary approach considers unhealthy nutrition, lack of sun and clean water, excess toxins, lack of normal physical activity, sleep disturbances and chronic stress as the direct causes of the disease.
Nail psoriasis and psoriatic arthritis are linked
The connection between nail damage and psoriatic arthritis has been known for a long time.
Based on the observations, the scientists found that psoriatic arthritis is accompanied by nail damage in nine out of ten cases.
But the mechanism of this connection has not been fully studied. However, the authors of several studies, for example the Leeds Institute of Molecular Medicine (UK), have tried to explain this connection beyond the concept of immune inflammation.
According to them, the fact is that the joint of the finger is located near the nail and is anatomically associated with it.
Therefore, the microtraumas and Kebner's phenomenon that cause primary joint inflammation - psoriatic arthritis - also cause secondary pathological changes in the nearest nail.
This is why psoriatic arthritis is associated with nail damage so often.
%20of%20the%20toes.jpg)
Therefore, the symptoms of nail psoriasis are often indicative of psoriatic arthritis.
Let's now look at the main myths that accompany this disease and how they are dangerous.
Myth 1: Nail psoriasis is rare.
Not exactly. Apparently, with psoriasis, nails suffer very often.
According to various sources, nail psoriasis occurs in the range of 6% to 82% of cases of psoriasis vulgaris. Such a wide spread in the assessment of the prevalence of this pathology is explained by problems in its accounting. Medical statistics record visits to doctors primarily by patients with a vulgar shape, and secondly, the focus is on the nails. In scientific research, cases of nail psoriasis are also usually studied only in addition to the main object of interest - psoriasis with skin lesions.
However, numerous publications state this
up to 80-90% of patients with psoriasis vulgaris reported recurrent nail damage.
And also that nail psoriasis occurs in 90% of patients with psoriatic arthritis and scalp psoriasis.
It should be noted that adults usually suffer from this form of the disease.
According to various sources, nails in children are affected in about 7-37% of psoriasis cases. Unfortunately, the manifestations of psoriasis on a child's nails are often not given due importance. Parents or doctors believe that this is a variant of the norm or a consequence of trauma, or they simply do not notice it due to the mild severity of the symptoms.
Myth 2: Recognizing nail psoriasis from symptoms is easy
In fact, not always. The fact is that
the nail is able to respond to various diseases only with a limited number of symptoms. Therefore, the manifestations of various diseases on the nails may look the same.
Of course, nail psoriasis can be suspected if the patient has severe symptoms of psoriasis vulgaris. However, nail lesions can be minor compared to skin lesions and can be easily ignored by a doctor.
Usually, the more active psoriasis is on the skin, the more severe the damage to the nails.
First of all, the nails are affected.
And it is also important to know that in 5% of cases, nails can be the only initial manifestation of psoriasis. That is, the classic manifestations of psoriasis on the skin can be completely absent.
The appearance of nail psoriasis depends on where the pathological changes originate: in the matrix or in the nail bed.
The source of symptoms - matrix or bed - is important to consider when choosing a treatment. Therefore, it is necessary to define it correctly.
Symptoms that originate in the nail matrix are:
- symptom of thimble,
- white spots and dots (leukonychia),
- red spots on the hole,
- crumbling nails.
Although the cause of these symptoms is at the level of the matrix, as the nail grows, pathological changes appear on the nail plate.
Symptoms, the cause of which is in the nail bed, are:
- detachment of the nail (onycholysis),
- longitudinal hemorrhage,
- subungual hyperkeratosis,
- symptom of an oil stain.
Next, we will focus on each symptom separately. And let's start with the manifestations that originate in the matrix.
Thimble symptom
The symptom of a thimble appears on the surface of the nail plate with holes or pits, which look like depressions in a thimble.
Such defects mainly occur on the nails, but rarely appear on the feet. As the nail grows, the cavities move from the crease of the nail to the edge of the nail plate.
Pits in nail psoriasis are usually deep, large, and chaotic. They arise due to the peeling of loose groups of cells from the surface of the nail, in which division and keratinization are impaired.

The more severe the psoriasis, the more often the thimble symptom occurs.
However, it should be borne in mind that, in addition to psoriasis, cavities on the nails are also characteristic of alopecia areata (alopecia), eczema, dermatitis, and can also occur, for example, with a fungal infection.
Counting the total number of cavities on all nails will help make the correct diagnosis.
- Less than 20 - not typical of psoriasis,
- 20 to 60 - psoriasis can be suspected,
- more than 60 - confirms the diagnosis of psoriasis.
White patches (leukonychia)
Leukonychia is a symptom that manifests itself as white spots or dots on the nails.

With leukonychia (from the Greek.leukós- white andonychos- nail), in contrast to the superficial cavities in the symptom of a thimble, cells with impaired division and keratinization are found in the thickness of the nail plate. At the same time, the nail surface remains smooth. And the white color of the spots comes from the reflection of light from the clusters of dislocated cells.
However, some studies suggest that leukonychia is so common in healthy people that it is not a characteristic symptom of psoriasis. For example, a manicure injury can cause leukonychia.
Crumbling nails
When the superficial pits (symptom of the thimble) and the deep areas of leukonychia (white spots) come together, the nails begin to crumble.

Typically, nail crumbling occurs with long-term nail psoriasis.
And the more intense the inflammation of the nail matrix, the more the nail plate is destroyed. In severe cases, the nail can completely collapse and fall out.
Red dots on the orbit of the nail
Apparently, red spots in the area of the hole and its general redness occur due to increased blood flow to the vessels under the nail.
In addition, red spots are formed on the hole due to a violation of the structure of the nail plate itself - it becomes more transparent and thinner. And because of this, firstly, the vessels become better visible, and secondly, the thin nail plate exerts less pressure on the vessels below and is more filled with blood.

Thinning of the nail plate can also cause redness of the entire nail bed.
Detachment of the nail (onycholysis)
Now let's consider the symptoms, the source of which is the nail bed.
Onycholysis is the separation of the nail plate from the bed due to the accumulation of cells under the nail with reduced division and keratinization.

Onycholysis itself (from the Greek.onychos- nail eλύσις- separation) is not necessarily a sign of psoriasis and can develop, for example, as a result of an injury to the nail.
Initially, the loss of contact between the nail and the bed occurs in the area of hyponychia, along the outer edge of the nail plate. Then onycholysis spreads to the fold of the nail in the form of a semicircular line. The exfoliation area turns white due to the accumulation of air under the nail.
A reddish border (scientifically erythema) along the edge of onycholysis, which is usually visible on the fingers, is characteristic of psoriasis and helps make the correct diagnosis.

With prolonged onycholysis, the nail bed loses its properties and the new growing nail, most likely, will not be able to attach normally. Therefore, even with a complete renewal of the nail plate, onycholysis often persists.
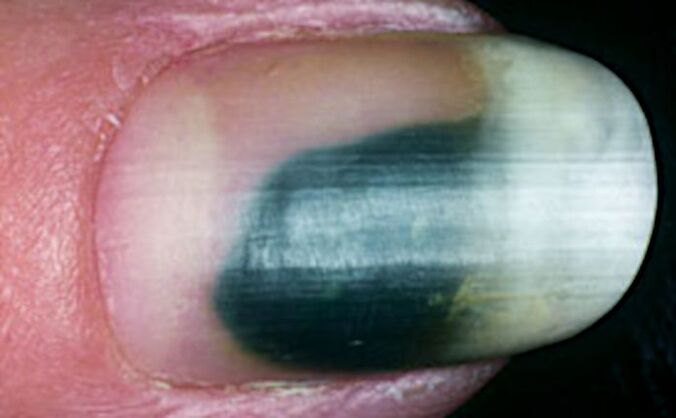
Due to the fact that onycholysis facilitates the penetration of bacteria and fungi, the infection can join. This sometimes leads to the discoloration of the nail. For example, a greenish color can occur when bacteria attach themselvesPseudomonas aeruginosa(Pseudomonas aeruginosa) and others.
Longitudinal subungual hemorrhage
Longitudinal subungual hemorrhages occur in the nail bed and appear as 1-3mm long dark red lines.
Increased blood flow and edema in the area of inflammation of the nail bed lead to rupture of the capillaries, which manifests itself in the form of such hemorrhages.

Due to the peculiarities of the blood supply, most hemorrhages occur closer to the free edge of the nail, in the area of hyponychia.
Subungual hyperkeratosis
Subungual hyperkeratosis is a buildup of dead cells under the outside of the nail plate.

With psoriasis, subungual hyperkeratosis (from the Greek.hyper- excessively ekeras- horn) is generally silvery white in color, but can also be yellow. And when the infection joins, it can become, for example, greenish or brown.
The more the nail is raised above the nail bed, the greater the activity of the pathological process.
On the fingers, subungual hyperkeratosis usually manifests as loose layers under the nail plate. On the legs, these masses are firmly welded with a thickened nail.

Also, psoriasis with toenail lesions is characterized by a combination of subungual hyperkeratosis with onycholysis (separation of the nail).
Oil spot symptom
The symptom of an oil spot appears under the nail plate in patches of yellow-red (salmon) color.
They occur on the nail bed closest to the nail crease and move to the edge of the nail as it grows.

The cause of this symptom is inflammation of the nail bed with expansion of capillaries and an accumulation of cells involved in inflammation, as well as cells with impaired division and keratinization.
Oil stains come in a variety of shapes and sizes. They can be found both in the center of the nail and on the edge, near the onycholysis area.
Myth 3: Nail psoriasis is just a cosmetic problem.
In reality this is not true. Although over 90% of patients report unsightly psoriasis nails, this isn't just a cosmetic issue.
According to various studies, nail psoriasis significantly reduces the quality of life of patients:
- 52% of patients also complain of pain,
- 59% - for problems in daily activities,
- 56% - for difficulties at home e
- 48% - due to difficulties at work.

Therefore, it is very important to make the correct diagnosis and start treatment as soon as possible, as improving the condition of the nails significantly improves the quality of life of patients with psoriasis.
Myth 4: Nail psoriasis is not dangerous
In fact, this is not the case. Speaking above about the causes of this form of the disease, we have already written about it
nail psoriasis is an important symptom of psoriatic arthritis.
It is important to keep in mind that the external manifestations of arthritis can be completely absent. In this case, we can talk not only about the fact that the joints of the fingers and toes are affected, but the joints of the spine and pelvic bones can also be involved.
You can check your joints for arthritis with ultrasound (ultrasound) or magnetic resonance imaging (MRI).

Although there are no obvious symptoms of arthritis, but there are manifestations of nail psoriasis, it is very important to make sure that all joints are in order.
And then regularly monitor the condition of the joints. Otherwise, psoriatic arthritis can be easily lost! Late diagnosis will lead to late treatment and, consequently, irreversible joint damage and disability.
Therefore, if the doctor has not ordered a research on insurance, citing the absence of visible signs of arthritis, you should personally contact the clinic and undergo, for example, a paid ultrasound.
How to diagnose nail psoriasis
It is important to be able to recognize the numerous symptoms of nail psoriasis, which we have described above, as they help establish the correct diagnosis. But because the nail changes characteristic of psoriasis can also occur in other diseases, it can be difficult to make a correct diagnosis right away.

In this case, having multiple symptoms on different nails at the same time can help in the diagnosis.
The important signs of psoriasis on the nails are:
- a symptom of a thimble: more than 20 dimples on all fingernails indicate the possibility of psoriasis and more than 60 dimples confirm the diagnosis of psoriasis,
- detachment of the nail (onycholysis) with a reddish border around the edge,
- oil (salmon) stains on the nail bed.
Difficulty in diagnosing nail psoriasis from a single symptom
It is especially difficult to diagnose nail psoriasis if it presents with only one symptom.
For example, if you only have onycholysis on the hands or only subungual hyperkeratosis on the arms and / or legs.
The only method for making a reliable diagnosis in isolated onycholysis (nail detachment) is probably the study of hyponychia using a special microscope - a dermatoscope.
For this, a high-magnification video dermatoscope is used. Please note that the handheld dermatoscope does not provide the required magnification. What you need is a video dermatoscope with a magnification of at least 40 times. Then the dilated capillary loops characteristic of psoriasis become visible.

With isolated subungual hyperkeratosis, the likelihood of psoriasis is high if the buildup of scales under the nail is whitish-silver in color, as well as if all fingernails or toenails are affected.
Psoriasis or nail fungus?
About 30% of nail psoriasis patients also have a fungal infection - scientifically onychomycosis.
Outwardly, hyperkeratosis and onycholysis (separation of the nail) in psoriasis can resemble the manifestations of a fungal infection. Therefore, it can be difficult to carry out differential diagnostics, that is, to identify the true cause of changes in the nail plate.
Also, both psoriasis and fungi can affect the same nails at the same time. Most often it occurs on the toes and is mainly characteristic of older patients.
Also, with a fungal infection, one or both of the toenails are often affected. In psoriasis, as a rule, several nails are affected at the same time.

The following symptoms speak in favor of psoriasis:
- oil stains and / or a symptom of a thimble on the nails,
- signs of psoriasis on the scalp and / or large skin folds,
- periodic remission and exacerbation of nail damage.
In favor of onychomycosis they say:
- longitudinal stripes on the affected nail,
- detection of fungi during microscopic examination of a potassium hydroxide-treated scraping from an affected nail (KOH test),
- positive culture for fungi.
In general, on the basis of external manifestations alone, it is impossible to completely exclude fungal infection of the nails in patients with psoriasis.
It should also be remembered that a fungal infection can cause Kebner's phenomenon on the nail and surrounding skin, resulting in psoriasis symptoms. So anyway
It is helpful to go to a mycologist and do a fungal test and, if found, start antifungal therapy.
Important results and what to do
Let's summarize important information about nail psoriasis and its symptoms.
Diagnostic features:
- Nail psoriasis is very common but often goes undetected.
- Manifestations of nail psoriasis can be minor, so even experts often do not pay attention.
- In 5% of cases, nail damage may be the only symptom of incipient psoriasis.
- The manifestations of different diseases on the nails may look the same, which further complicates the diagnosis.
The main manifestations of nail psoriasis:
- a symptom of a thimble - pits on the nail,
- white spots,
- crumbling nails
- red dots in the hole area,
- detachment of the nail,
- longitudinal subungual hemorrhage,
- subungual hyperkeratosis - loose clusters under the nail,
- symptom of an oil stain.
Psoriasis and fungi:
- Often, nail psoriasis is accompanied by a fungal infection.
- To unambiguously exclude it, you need to contact a mycologist and conduct additional research.
Nail psoriasis and psoriatic arthritis:
- Nail psoriasis is a common companion of psoriatic arthritis.
- It is important to detect pathological changes in the joints as early as possible to start treatment on time and avoid irreversible complications and disabilities.
- Even if there are no external symptoms of arthritis, but nail psoriasis is detected, it is necessary to undergo an examination of the joints using ultrasound or MRI.
























